by David Piskulic, DPT, SCS, ATC/L
St Louis Children's Hospital Physical Therapy
Ankle sprains are one of the most common injuries in sports
participation. In fact, the ankle
accounts for about 1/3rd of all sport-related injuries. In their lifetime, 1 in 5 individuals who are
physically active will sustain a lateral ankle sprain, which is when the foot
turns in and the ligaments on the outside of the ankle are either damaged or
torn. Incidence of these ankle sprains
is highest in our young athletes, between 15-19 years. While the incidence of these injuries is well
known, proper rehabilitation of the injury and knowing when to get back to
sports participation can be difficult to determine.
How Do I
Start Care for an Ankle Sprain?
After your athlete sustains an ankle injury, observe for
common signs and symptoms: localized pain, swelling that builds up and may lead
to discoloration, a popping sound during the injury, and difficulty moving the
ankle or foot. Be especially aware of
difficulty bearing weight on the leg or even difficulty walking, as this may be
a sign of a more severe ankle sprain or fracture. If you suspect a severe injury, follow-up
with your physician for a full evaluation.
Once an ankle sprain is determined, the old method of rest,
ice, compression, and elevation (often referred to as “R.I.C.E.”) still stands
tried and true. The athlete should rest
from activity, ice the area of pain for up to 15-20 minutes, maintain
compression with a wrap, and elevate the ankle above the level of the
heart. All of these initial treatments
will help with overall circulation and decrease excessive swelling. More severe sprains may require use of a boot
or air-cast that can be acquired from and applied by your physician.
Figure 1 : Examples of wraps and bracing to treat ankle sprains.
When Can
I Move My Ankle?
While you initially want to protect the injured ankle ligaments
and restrict ankle movement to let them heal, light range of motion exercises
can help prevent stiffness and improve circulation to allow proper blood flow
for healing and reduction of swelling.
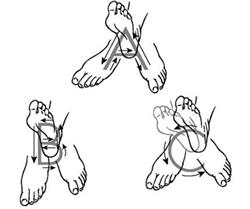
Some simple exercises are completing the “ankle alphabet”. The athlete will “draw” letters of the
alphabet with their big toe, moving their ankle through pain-free range of
motion. This can be accomplished by starting
with small letters and gradually making bigger letters once pain improves.
Figure 2 : Examples of "ankle alphabet" exercises
When Can
I Walk?
Early
weight bearing has been linked to improved outcomes in rehabilitation of ankle
sprains. It is important for the athlete
to “normalize” their walking pattern and to have their heel touch the ground
first with their toes forward, then roll through their step and gently push off
from their toes. If use of a larger boot
or brace limits ankle mobility, have the athlete roll through their step with
their toes forward as much as possible. If
the athlete is having difficulty pushing off from their toes during walking,
they may benefit from completing a heel raise exercise. The athlete can complete the exercise on both
legs at the same time and then progress to single leg heel raises as their
strength improves.
Figure 3 : Example of proper walking mechanics at the foot and ankle
Figure 4 : Example of a heel raise exercise with heels elevated
In addition to the athlete having a normalized walking
pattern, they should also work on balance exercises to assist with stabilizing
the ankle. Several studies have been
done on specific types of exercises, use of equipment and special supplies, but
the main conclusion these studies have is that any type of exercises that
challenge an athlete’s single leg balance, such as balancing on uneven
surfaces, promote improvement in overall stability of the ankle joint. This can be accomplished by having the
athlete balance on 1 leg on a flat surface while pain free for up to 30
seconds. When the athlete reports no
pain with these exercises, they can start single leg balancing on uneven
surfaces, such as thick carpeting or a couch cushion, and practice sport
specific drills, such as throwing and catching a ball. These types of balances programs are even
recommended as a pre-season work-out and have been correlated to decreased
incidence of injuries among athletes.
When Can
I Play Sports Again?
This is usually the most important question asked after sustaining
an injury, not only by the patient but by the parents as well. And don’t worry, parents, clinicians want
your young athlete to return to their sport or activity as soon as
possible! We just want to make sure
they’re safe and healthy to do so.
Some tests to complete with the athlete are single leg
balancing, pain-free walking and running without favoring their injured leg,
performance of sport specific skills without any form of contact from other
players or teammates, and equal performance of jumping and hopping on each leg. Your rehabilitation specialist of choice should
be able to help your athlete in finding exercises and activities for them to
complete to properly train their injured ankle and get them fully prepared to
return to their sport.
How Do I
Keep From Getting Injured Again?
In a perfect world, everyone would be able to
participate in their own sport or activity free from aches, pains, and
injuries. However injuries are very much
a part of the sports world and unfortunately will continue to occur despite our
best efforts. That being said, there are
still many things to do to avoid a higher incidence of future injury. This includes several aspects of sports
training, including continued training in balance exercises throughout sports
participation, completion of a thorough return to sports test with your medical
provider, and continued use of ankle support with use of a functional lace-up
ankle brace or taping. These have been
found to reduce the incidence of ankle sprains when returning to sports
following injury. Consult your
physician, physical therapist, or athletic trainer for their recommendations on
functional bracing and for assistance with application of ankle taping.